CORNEA TRANSPLANTATION
Cornea Transplantation Process and Its Importance
Various health problems encountered throughout life can cause different levels of damage to the tissues or organs in our body. Although there are various methods especially in the treatment of organ failures, the most effective solution in end-stage tissue and organ failures is the transplantation of the tissue or organ from the donor to the recipient. In this context, corneal transplantation is an important treatment method for the renewal of corneal tissue, which is a critical part of the eye.
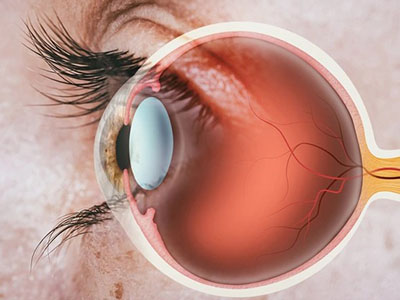
What is Cornea?
The cornea is a transparent, dome-shaped tissue located in the front part of the eyeball. It is the region where the light required to perceive the image is first transmitted to the eye and where the light is refracted, providing the connection between the outside world and the eye. The cornea directs the refracted light through the pupil to the inside of the eye. Here, the eye lens refracts the light a second time and focuses it on the yellow spot, which creates a clear image on the retina. The image formed in the macular dot is transferred to the nerve cells by receptor cells and transmitted to the visual center of the brain. A healthy cornea is needed to obtain a clear image. The cornea is not directly supplied by blood vessels; instead, it receives nutrients and oxygen by diffusion from the body fluid in the space between the iris and cornea.
What is Cornea Transplantation?
Corneal transplantation refers to the process of replacing the damaged cornea, whose structure is damaged due to various health problems, with healthy corneal tissue taken from the donor body. In this process, the entire corneal tissue or only the upper layer can be transplanted. In some selected cases, artificial corneal tissues can also be used.
Donors for cornea transplantation are usually selected from deceased individuals. However, people whose disease history or health status is unclear or who have died for unknown reasons are not accepted as donors. These conditions may increase the risk of infection of the cornea and may also be affected by the donor's existing chronic diseases. Since cornea does not require tissue compatibility like kidney or liver, transplantation is easier than other organs.
Feasibility of Cornea Transplantation
Transplantation of some or all of the corneal tissue is often necessary in cases of irreversibly damaged cornea. Corneal transplantation may be considered for individuals with the following health problems:
Keratoconus: Deformity of the cornea caused by congenital or subsequent curving outwards.
Fuchs Dystrophy: Congenital disorders in the corneal structure.
Corneal Thinning or Tear: Thinning or damage of corneal tissue.
Infection or Trauma: Corneal damage caused by physical factors.
Corneal Edema: Loss of tissue or function in the cornea due to cessation of oxygen supply.
Corneal Ulcers That Do Not Respond to Medical Treatment: Advanced corneal ulcers.
Previous Surgical Procedures: Irreversible damage caused by surgical interventions on the eye
Corneal transplantation is generally a successful surgical procedure; However, it may involve some risks and complications. For this reason, it is extremely important that the procedure be performed by experienced healthcare personnel in centers specialized in the field. Cornea transplantation is performed by surgeons specialized in eye diseases (ophthalmology).
What is the Cornea Transplantation Process?
Cornea transplantation is planned with the evaluation of the specialist doctor, depending on the patient's specific condition and underlying health problems. This process can be accomplished by various methods:
1. Full Thickness Cornea Transplantation (Penetrating Keratoplasty)
This method involves removing all layers of the cornea and replacing them with all layers of a suitable donor cornea. The transplanted tissue is placed with small stitches and monitored by the surgeon during the postoperative period.
2. Endothelial Keratoplasty
In this method, healthy upper layers are preserved while diseased lower layers are removed. The damaged parts of Descemet's membrane, which is located under the cornea and plays an important role in the healing process, are replaced with tissue taken from the donor. If the procedure covers one-third of the cornea, it is called "Descemet Stripping Endothelial Keratoplasty" (DSEK), and if a thinner layer is removed, it is called "Descemet Membrane Endothelial Keratoplasty" (DMEK).
3. Anterior Lamellar Keratoplasti (ALK)
This method is a surgical procedure in which the diseased upper layers are removed and the lower layers are preserved. In case of removal of deep layers, the terms "Deep Anterior Lamellar Keratoplasty" (DALK) are used, and for more superficial procedures, the terms "Superficial Anterior Lamellar Keratoplasty" (SALK) are used. The tissue taken from the donor is transplanted to replace the removed part.
4. Artificial Cornea Transplantation (Keratoprosthesis)
In certain cases, if the cornea from the donor cannot be used, an artificial cornea produced in a laboratory can be transplanted.
Cornea transplantation can be done under general or local anesthesia and is usually performed on one eye at a time. In the postoperative period, drug treatments are administered to control pain and prevent the risk of infection. During the healing process, side effects such as eye pain, redness, sensitivity to light and watering may occur. By using protective equipment, the transplanted eye is protected from external factors.
After the procedure, patients' vision is significantly improved and vision loss is prevented. However, vision may deteriorate over time as the new cornea adapts to the body; In this case, additional treatment or surgical intervention may be required.
Risks of Cornea Transplantation
Corneal transplant carries the risk of various complications. However, this procedure, which has been successfully performed worldwide, is often associated with rare complications. The transplanted corneal tissue can function healthily for approximately 10 years.
In this regard, the following health problems may arise during or after the surgical procedure:
eye infections
Increased intraocular pressure (glaucoma)
Non-healing or problematic healing of the surgical site
Rejection or failure to nourish the transplanted cornea
Bleeding
Damage to eye tissues, retina problems or retinal detachment
Development of refractive errors such as astigmatism, distance or near vision disorders in the eye after surgery
After transplantation, corneal tissue may be perceived as foreign tissue by the body or may be damaged due to insufficient nutrition and oxygen support. This condition may present with symptoms such as vision loss, eye pain, redness, and sensitivity to light.

